Endoscopic Discectomy: A Minimally Invasive Solution for Disc Herniation
Endoscopic Spine Surgery, or discectomy, is a cutting-edge surgical procedure used to treat disc herniation in the spine. This minimally invasive technique offers several advantages over traditional open surgery, including smaller incisions, reduced tissue damage, faster recovery times, and less postoperative pain. This webpage serves as a comprehensive guide to endoscopic discectomy, providing valuable information on its indications, procedure, benefits, and potential risks.
What is Endoscopic Discectomy?
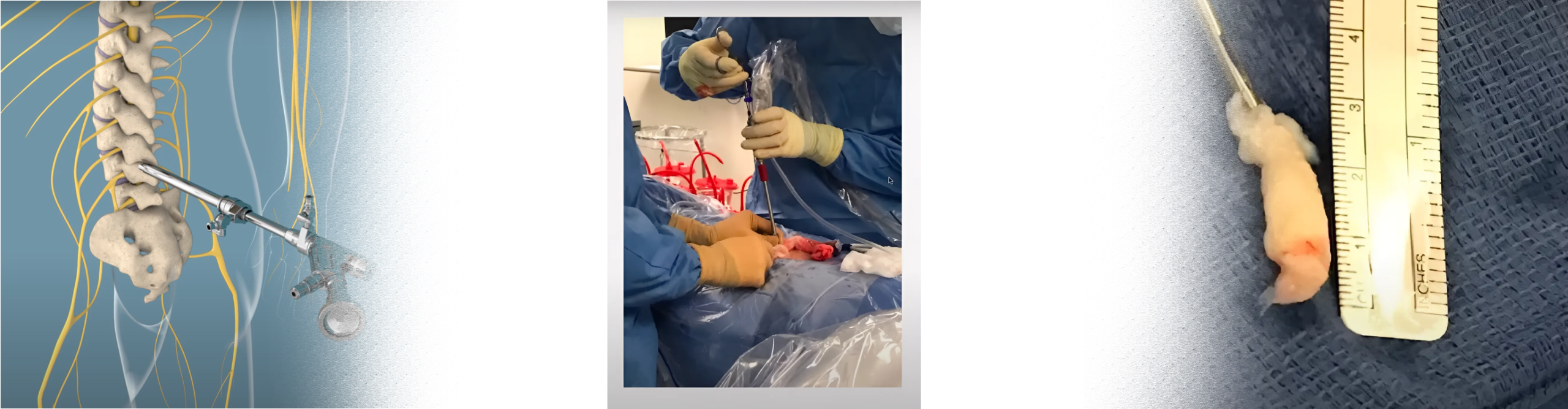
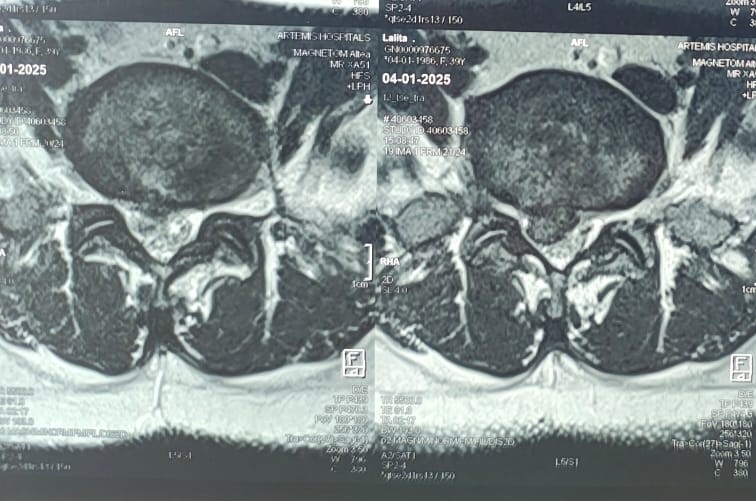
Endoscopic discectomy is a minimally invasive surgical procedure used to treat disc herniation in the lumbar spine. The procedure involves accessing the herniated disc through a small incision in the back using an endoscope, a thin tube with a camera and surgical instruments attached. By visualizing the herniated disc on a monitor, the surgeon can precisely remove the herniated portion of the disc, relieving pressure on the spinal nerves and alleviating symptoms such as pain, numbness, and weakness.
Indications for Endoscopic Discectomy:
Endoscopic discectomy may be recommended for individuals with:
– Lumbar disc herniation causing radicular symptoms (sciatica)
– Persistent or severe back and leg pain that does not respond to conservative treatments such as medication or physical therapy
– Disc herniation compressing spinal nerves, leading to neurological symptoms such as weakness, numbness, or tingling in the legs
– Recurrent disc herniation after previous discectomy surgery
Procedure:
Endoscopic discectomy is typically performed under local anesthesia with sedation and involves the following steps:
1. Patient Positioning: The patient is positioned face down on a specialized operating table, allowing access to the lumbar spine.
2. Incision: A small incision (usually less than one cm) is made in the back, directly over the affected disc.
3. Endoscope Insertion: The endoscope is inserted through the incision and guided to the herniated disc under fluoroscopic guidance.
4. Visualization: The surgeon visualizes the herniated disc and surrounding structures on a monitor connected to the endoscope.
5. Discectomy: Using specialized instruments, the surgeon removes the herniated portion of the disc, relieving pressure on the spinal nerves.
6. Closure: No uterus or clips are required. The incision is closed with a surgical glue, and a sterile dressing is applied to the surgical site.
Benefits of Endoscopic Discectomy:
Endoscopic discectomy offers several advantages over traditional open surgery, including:
– Smaller incisions and reduced tissue damage
– Faster recovery times and shorter hospital stays
– Early return to work
– Less postoperative pain and reliance on pain medication
– Preservation of spinal stability and range of motion
– Minimal scarring and improved cosmetic outcomes
Conclusion:
Endoscopic discectomy is a highly effective and minimally invasive surgical procedure for treating lumbar disc herniation, providing significant relief from pain and other symptoms while minimizing surgical trauma and downtime. If you are experiencing symptoms of a herniated disc, consult with a spine specialist to determine if endoscopic discectomy may be an appropriate treatment option for you. With proper evaluation and surgical care, many individuals can achieve significant improvement in pain and function, leading to a better quality of life.
This webpage serves as a comprehensive resource for individuals seeking information about endoscopic discectomy, empowering them to make informed decisions about their spine health and treatment options.




