Spinal Infections: Understanding, Diagnosis, and Treatment
What Are Spinal Infections?
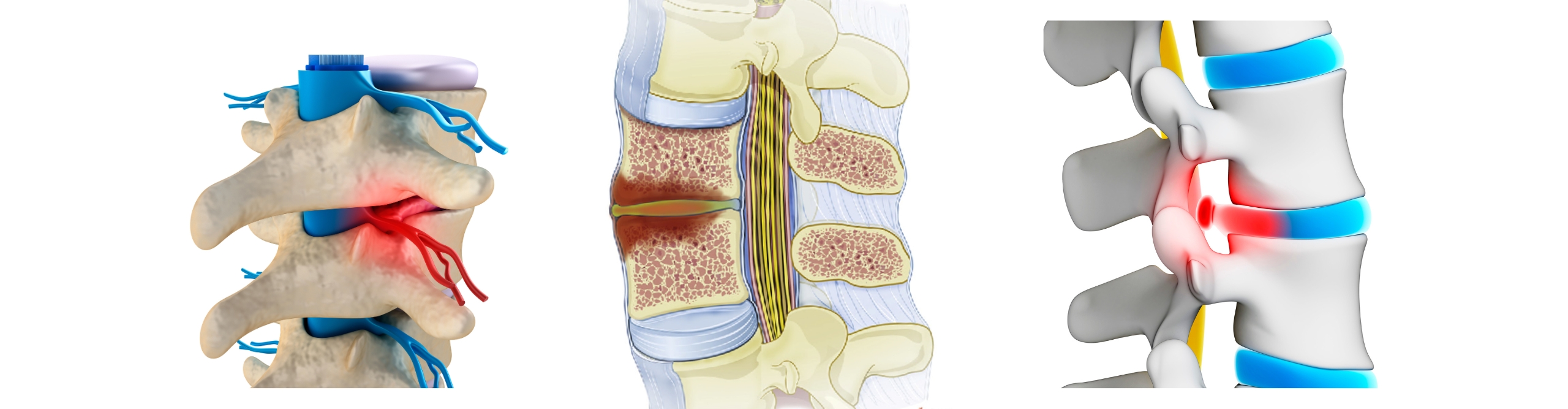
Spinal infections, also known as vertebral osteomyelitis, are infections that affect the vertebrae (bones of the spine), intervertebral discs, or the surrounding spinal tissues. These infections can be caused by bacteria, fungi, or, in rare cases, viruses. Spinal infections are serious medical conditions that require prompt diagnosis and treatment to prevent severe complications.
Types of Spinal Infections
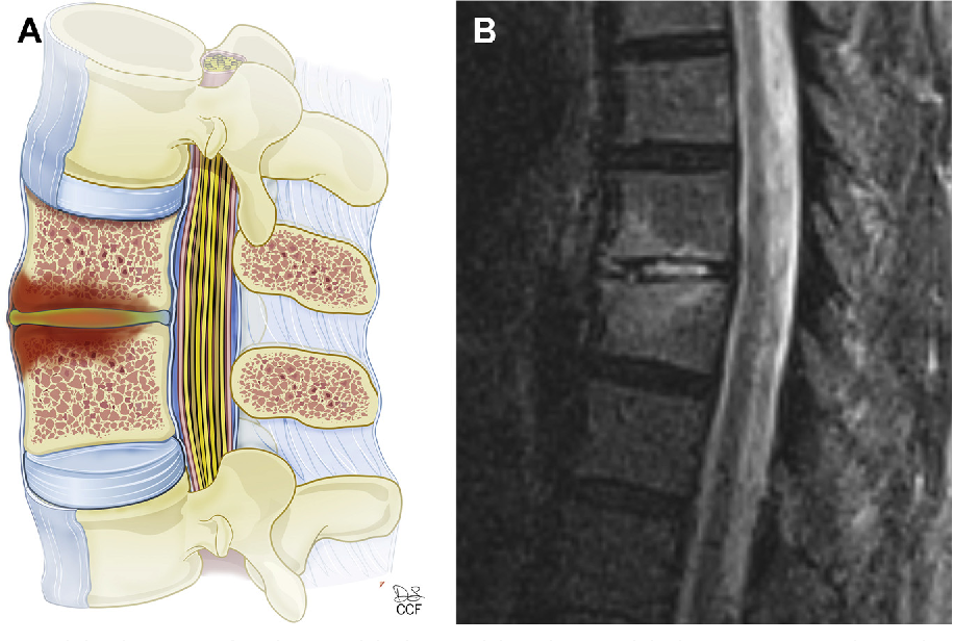
1. Vertebral Osteomyelitis:
– Infection of the vertebral bones.
– Commonly caused by bacteria such as Staphylococcus aureus.
2. Discitis:
– Infection of the intervertebral discs.
– Can occur in isolation or alongside vertebral osteomyelitis.
3. Epidural Abscess:
– Accumulation of pus between the spinal cord and the vertebrae.
– Requires urgent medical intervention.
4. Spinal Tuberculosis (Pott’s Disease):
– Caused by Mycobacterium tuberculosis.
– Often affects the thoracic and lumbar spine.
Causes and Risk Factors
1. Infectious Agents:
– Bacteria: The most common cause, including Staphylococcus aureus, Escherichia coli, and Streptococcus species.
– Fungi: Less common but can include Candida and Aspergillus species.
– Viruses: Rarely cause spinal infections but can occur in immunocompromised individuals.
2. Risk Factors:
– Immunosuppression: Conditions like HIV/AIDS, diabetes, or use of immunosuppressive medications.
– Intravenous Drug Use: Increases the risk of bloodstream infections that can spread to the spine.
– Chronic Conditions: Diabetes, chronic kidney disease, and other chronic illnesses can predispose individuals to infections.
– Infections in Other Body Parts: Infections such as urinary tract infections or skin infections can spread to the spine through the bloodstream.
Symptoms
– Severe Back Pain: Persistent and often worse at night.
– Fever and Chills: Indicative of an ongoing infection.
– Neurological Symptoms: Numbness, weakness, or paralysis in severe cases if the infection compresses the spinal cord or nerves.
– Localized Tenderness: Pain when the affected area of the spine is pressed.
– Loss of Appetite and Weight Loss: Common in chronic infections.
Diagnosis
1. Medical History and Physical Examination:
– Detailed history to identify risk factors and symptoms.
– Physical examination to locate pain and neurological deficits.
2. Laboratory Tests:
– Blood tests including complete blood count (CBC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) to detect inflammation and infection.
– Blood cultures to identify the causative organism.
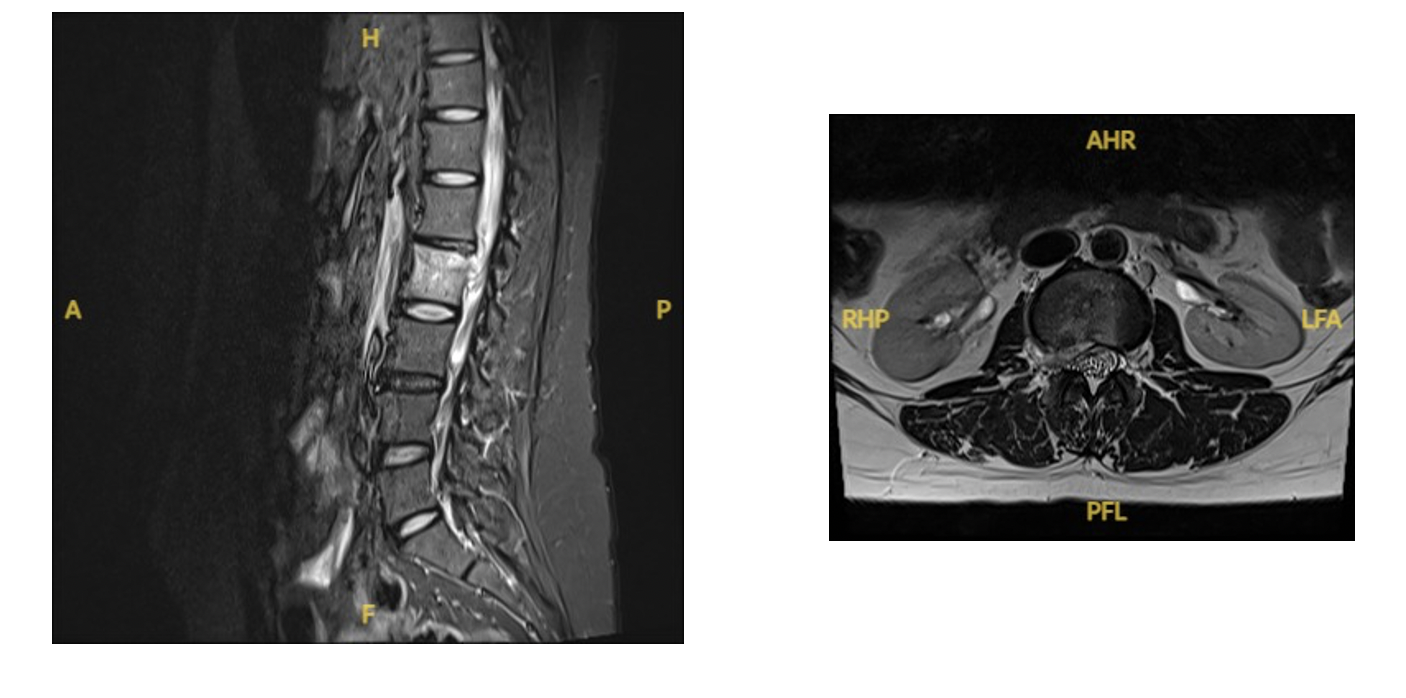
3. Imaging Studies:
– X-rays: Initial imaging to detect bone destruction.
– MRI: The gold standard for diagnosing spinal infections, providing detailed images of the spine and surrounding tissues.
– CT Scan: Used if MRI is contraindicated.
– Bone Scintigraphy: Can help in early detection when other imaging is inconclusive.
4. Biopsy:
– Percutaneous needle biopsy or open biopsy to obtain tissue samples for microbiological and histopathological examination.
Treatment
1. Antibiotic or Antifungal Therapy:
– Long-term intravenous antibiotics or antifungal medications based on the identified organism.
– Oral antibiotics may follow after initial IV therapy.
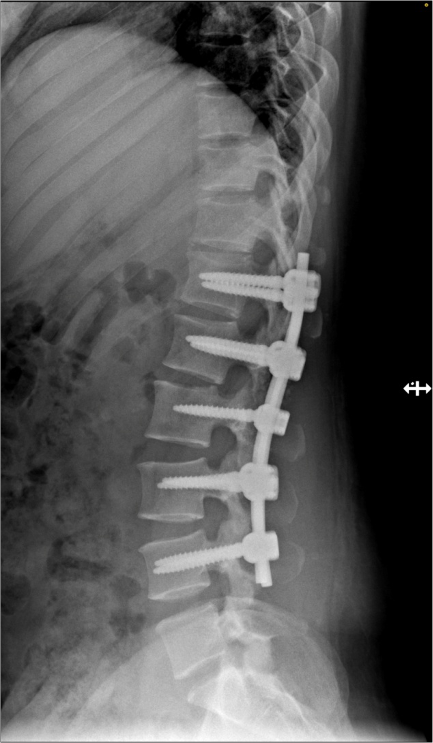
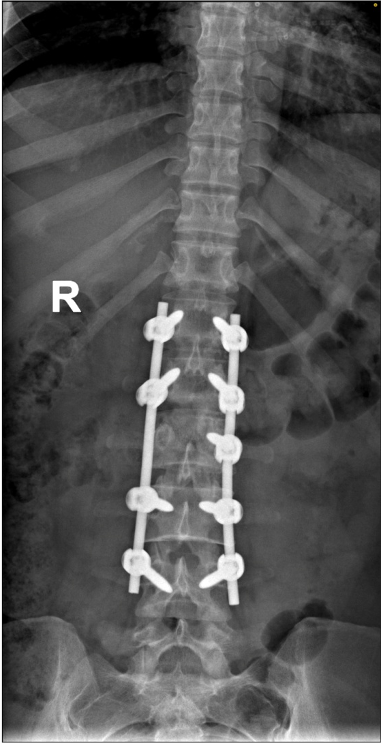
2. Surgical Intervention:
– Drainage: Abscesses may need to be drained surgically.
– Debridement: Removal of infected tissue and bone.
– Spinal Stabilization: In cases of spinal instability, surgical stabilization may be required.
3. Pain Management:
– Analgesics and anti-inflammatory medications to manage pain.
– Physical therapy may be recommended after initial infection control.
4. Supportive Care:
– Nutritional support and management of underlying conditions.
– Regular monitoring and follow-up to ensure infection resolution and prevent recurrence.
Prevention
1. Hygiene and Aseptic Techniques:
– Strict aseptic techniques during surgeries and medical procedures.
– Proper care of intravenous lines and catheters.
2. Managing Chronic Conditions:
– Effective management of diabetes, kidney disease, and other chronic illnesses to reduce infection risk.
3. Prompt Treatment of Infections:
– Early and appropriate treatment of infections elsewhere in the body to prevent spread to the spine.
4. Lifestyle Modifications:
– Avoiding intravenous drug use.
– Maintaining a healthy immune system through proper nutrition and regular exercise.
Conclusion:
Spinal infections are serious and potentially life-threatening conditions that require prompt diagnosis and treatment. Early recognition of symptoms, timely imaging, and appropriate antimicrobial therapy are crucial to prevent complications such as spinal deformity, chronic pain, and neurological deficits.




